Artificial Insemination (IUI)
Intrauterine insemination (IUI), also known as artificial insemination, is a fertility treatment that involves placing sperm directly into the uterus by the use of a catheter to increase the chances of fertilization and pregnancy.
The goal of IUI is to increase the number of motile sperm that reach a woman’s egg to increase the chances of fertilization. It is usually the first-line approach for couples seeking assisted reproductive treatment. Unlike IVF, IUI does not require the collection of eggs from the ovaries or fertilization outside of the body.
IUI is a relatively simple and painless outpatient procedure done at the time of peak ovulation.
As a leading fertility clinic in Raleigh, NC, Atlantic Reproductive Medicine specializes in personally tailored fertility treatments, including IUI. Our practice is known for providing comprehensive, individualized, and compassionate care.
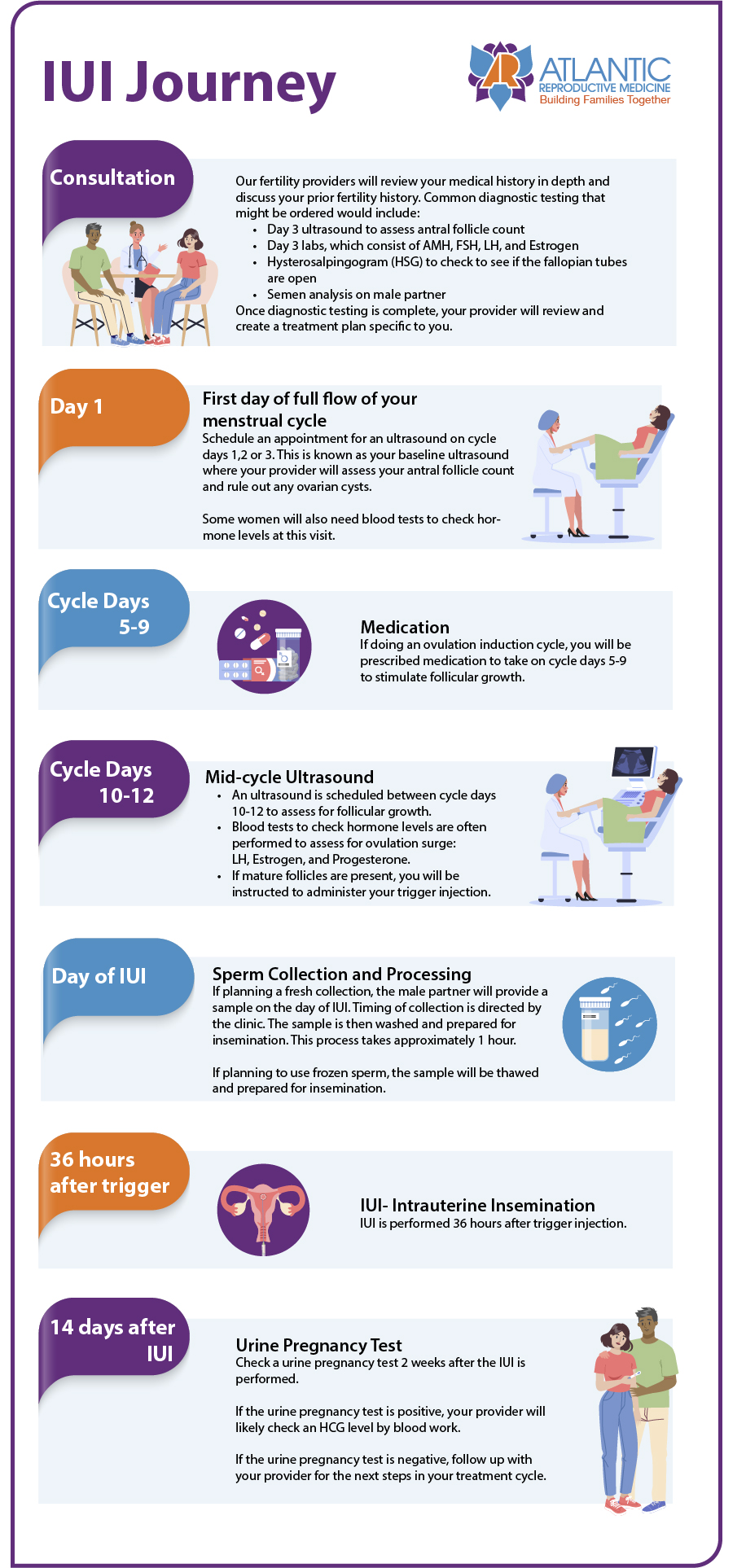
The IUI Process
Determining whether IUI is the right treatment for a patient starts with a medical consultation followed by diagnostic labs and tests. If a patient is a good candidate, a schedule is outlined that includes ultrasounds, medication timing, and the IUI treatment itself.
Sperm injected into the patient’s uterus can come from a partner or from a sperm donor. The sperm is always carefully washed in the andrology lab before being placed in the uterus. The lab processes the semen sample to remove any debris or unhealthy sperm, resulting in a final sample with highly motile sperm. The washing process also strips the semen of certain chemicals that can irritate the uterine tissue and reduce the IUI success rate.
After injection, the woman will spend a few minutes lying down and resting on the table to maximize the IUI success rate.
In the video below, Dr. David Walmer and Dr. Susannah Copland explain the IUI procedure. The transcript of their conversation is provided below the video.
Transcript of the video above on IUI
So when you meet with your patients to discuss the different fertility tools we offer, there are many options. There are a lot of different initials we throw around: IUI, INVOcell, and IVF. If we start with IUI, what do you tell your patients about IUI?
I start with IUI an acronym for intrauterine insemination. It’s for a selected group of patients. Sperm must get through two barriers to get into the upper reproductive tract. 90% of the sperm never get out of the vagina, and another 90% don’t get out of the cervix, so it’s one way of correcting low sperm numbers and enhancing that. It’s also a way of improving morphology because of the washing technique.
The IUI procedure
The technique involves putting the sperm through a gradient and separating the liquid portion of the sperm from the cells. The liquid-if even one drop of that got into the uterus, the woman would have severe reactions, fever, cramping. So, it’s important to separate those two things. But it can put the sperm directly into the uterus.
Once the sperm’s been processed, we load it into a catheter, and there’s a speculum in the vagina which exposes the cervix. You can thread the IUI catheter into the cervix, cervical canal, and upper cavity. When you deposit the sperm in the upper uterus, you’ve essentially increased the sperm count by a factor of 50-fold.
So you’ve washed the sperm, so the ejaculate is no longer there. You’ve bypassed one barrier that may be making it hard for that sperm to get to the woman’s eggs.
So, Susannah, how do you help your patients decide if they’re a good candidate for IUI?
Who is a good candidate for IUI
For IUI to work, you have to have a sperm sample that’s high enough that it can get through the washing process and still have a good number of sperm to put up into the uterus and open the Fallopian tubes because the only barrier that is going to be bypassed with IUI is the cervical mucus barrier. Because the sperm still has to swim up the Fallopian tube, and the egg still has to be grabbed by the Fallopian tube. They have to meet there and make their way back to the uterus. So when patients have completed their fertility workup, and they have a reasonable semen analysis, everything from normal to just a little bit abnormal, and they have open tubes, I talk to them about the data that shows that 1 in 4 couples will get pregnant, in up to three inseminations.
If they are pregnant in those three inseminations, we’ve reached the goal. If they’re not pregnant, then we know that we must have another barrier. Either the eggs and sperm aren’t finding each other, or the eggs and sperm are not interacting appropriately to achieve a fertilized embryo, or the fertilized embryo is not of the quality that is able to get to the uterus to make implantation to make an ongoing pregnancy. So, we would talk about other tools we could use, such as INVOcell or IVF.
Our Raleigh, NC Fertility Doctors grow families one relationship at a time, listening carefully to understand our patients’ goals, and working closely with all our patients to help them realize their goals
Over the years, Atlantic Reproductive Medicines has helped hundreds of patients grow their families through artificial insemination. Contact Atlantic Reproductive Medicine today to schedule an appointment to see if IUI is a good option for you. Patients from all over the Triangle, including Raleigh, Cary, Durham, Chapel Hill, Fayetteville, the country, and the world, come to our clinic for the best in female and male fertility treatments.
Basic Fertility Treatments

Controlled Ovarian Stimulation
Controlled Ovarian Stimulation, or hyperstimulation, is a mix of medications designed to stimulate follicle development, resulting in greater egg production in women. It’s frequently used as the first step of in vitro fertilization (IVF).

Intracytoplasmic Sperm Injection (ICSI)
Intracytoplasmic Sperm Injection, known as ICSI, is an option for couples battling male infertility. Atlantic Reproductive has successfully completed more than 5,000 cases of this procedure over the years.

Ovarian Reserve Testing
The number of eggs a woman has available is very important when assessing fertility and possible treatments. While there is an average number of eggs, every woman is different.
Advanced Fertility Treatments

INVOcell
The INVOcell, an FDA-approved gas-permeable vaginal culture device, allows women to incubate eggs and sperm themselves. This device decreases the cost of and increases access to fertility treatment.

IVF
One of the main fertility treatments we utilize at Atlantic Reproductive is in vitro fertilization (IVF), which involves fertilizing eggs with sperm outside the woman’s body.

IUI
Artificial insemination, also known as intrauterine insemination (IUI), is a technique that involves placing sperm inside the woman’s uterus with a catheter to achieve fertilization. Unlike IVF, artificial insemination does not require collecting eggs from the ovaries or fertilization outside the body.