
Vasectomy Reversal
Vasectomy reversal is a surgical procedure to undo a vasectomy. Male fertility is restored by reconnecting the tubes that sperm travel from the testicles to the semen.
About 15% of men who undergo a vasectomy regret it. About 5% will desire a reversal.
After a successful vasectomy reversal, a male’s sperm will again appear in the ejaculate, allowing for potential fertilization with a female egg.
Reversal success rates are high when a fellowship-trained surgeon does the surgery.
 “At Atlantic Reproductive Medicine, my patients receive the level of fertility expertise provided at top medical institutions, in a comfortable, private setting. Our vasectomy reversals are done on-site within our modern reproductive medicine center, in a male fertility operating room outfitted with a state-of-the-art operating microscope. We perform whatever reversal type is necessary, including both vasovasostomy (VV) and epididymovasostomy (EV) reversals, and the competitive, all-inclusive cost includes general anesthesia and simultaneous sperm banking of testicular sperm (TESE) in our unrivaled andrology laboratory.” – Matt Coward, MD
“At Atlantic Reproductive Medicine, my patients receive the level of fertility expertise provided at top medical institutions, in a comfortable, private setting. Our vasectomy reversals are done on-site within our modern reproductive medicine center, in a male fertility operating room outfitted with a state-of-the-art operating microscope. We perform whatever reversal type is necessary, including both vasovasostomy (VV) and epididymovasostomy (EV) reversals, and the competitive, all-inclusive cost includes general anesthesia and simultaneous sperm banking of testicular sperm (TESE) in our unrivaled andrology laboratory.” – Matt Coward, MD
ON THIS PAGE
- What factors determine whether a vasectomy reversal will be successful?
- What are the different types of vasectomy surgeries?
- What are vas deferens?
- What does a vasectomy reversal surgery entail?
- Choosing to extract and freeze sperm
- Are there risks involved with a vasectomy reversal?
- Post-surgery care
- Confirming surgery success
- What if the reverse surgery fails?
- The Atlantic Reproductive Difference
What factors determine whether a vasectomy reversal will be successful?
The most crucial factor determining reversal success is the experience of the surgeon. The surgeon should be a fellowship-trained reproductive urologist who can perform both a vasovasostomy (VV) and the more complex epididymovasostomy (EV) procedure.
- An expert urologist will have undergone 1-2 years of general surgery training followed by 4-5 years of urologic surgery residency training. After residency training, the reproductive urologist will have pursued another 1-2 years of additional sub-specialty training in microsurgery and male infertility surgery. The ideal reproductive urologist will have had 6-8 years of dedicated training operating on the male reproductive tract after medical school and before entering practice.
- The surgeon should use a modern, state-of-the-art operating microscope to aid visualization during the surgery. Vasectomy reversals without the use of an operating microscope are much more likely to fail.
- The vas deferens reconnections should be made in multiple layers using micro sutures that are finer than human hair.
A skilled surgeon like Atlantic Reproductive Medicine’s Dr. Matt Coward can reverse vasectomy on most men regardless of the time elapsed since the surgery, even significantly longer than ten years.
Dr. Matt Coward is a fellowship-trained reproductive urologist with over ten years of experience performing vasovasostomy (VV) and epididymovasostomy (EV) reversals using a state-of-the-art operating microscope. His surgeries are done in the setting of a reproductive medicine center, not a surgical center, which means savings and ease for his patients.
Dr. Coward performs his surgeries in a fully outfitted male fertility operating room with a dedicated anesthesia and nursing team. Patients receive the best of surgery skills and experience in a private, comfortable setting.
The total cost of a vasectomy reversal procedure at Atlantic Reproductive Medicine with Dr. Coward is $9,875, regardless of whether VV or EV is required on either or both sides. The price also includes general anesthesia and simultaneous sperm banking of testicular sperm (TESE).
What factors determine how much a vasectomy reversal costs
The cost of a vasectomy reversal depends on different factors:
- The surgery setting (hospital vs. private clinic). Reversals always cost more in hospitals and ambulatory surgical centers than in private clinics.
- The experience and surgical training of the surgeon. Non-urologists and non-fellowship trained doctors typically offer vasectomy reversals at a discount compared with fellowship-trained reproductive urologists because they often do not use a state-of-the-art operating microscope, they do not have the ability to perform an epididymovasostomy (EV) if necessary, and they do not offer sperm banking.
- The type of anesthesia provided. Some low-cost clinics will only provide oral sedation with local anesthesia injected into the surgical site. While this is feasible, it is uncomfortable for the patient, and patient movement can affect the ability to carefully place the sutures correctly. The gold standard anesthesia approach for a vasectomy reversal is with general anesthesia.
- The equipment used by the surgeon. A modern, state-of-the-art operating microscope should always be used to aid visualization. Low-cost clinics do not routinely use a modern microscope. In addition, many important supplies such as the microsutures required for a successful reconnection are expensive, and low-cost centers use fewer, and cheaper, sutures.
- Collaboration with an andrology laboratory. When a vasectomy reversal is not done in collaboration with an andrology laboratory, sperm banking is not provided as an option and may even be downplayed in importance.
- Sperm banking option. The total cost of the procedure can vary depending on whether or sperm banking is included with the cost of the reversal or is an additional fee.
Why you shouldn’t choose the cheapest option
Medical care should never be compromised, and the cheapest options for vasectomy reversal always either compromise on safety or success rates. Remember, the most important factor determining reversal success is the experience of the surgeon. The surgeon should be a fellowship-trained reproductive urologist who can perform both vasovasostomy (VV) and epididymovasostomy (EV). The surgeon should use a state-of-the-art operating microscope to aid visualization during the surgery, and general anesthesia should be provided for both patient safety and comfort.
Does insurance cover vasectomy reversal?
Only very rarely does medical insurance cover vasectomy reversal. For most patients, the procedure will be an out of pocket expense, however, the initial consult and any recommended blood work or imaging prior to the procedure are typically be covered.
There are two surgical options for vasectomy reversal:
- Vasovasostomy (VV): the severed ends of each vas deferens are sewn back together
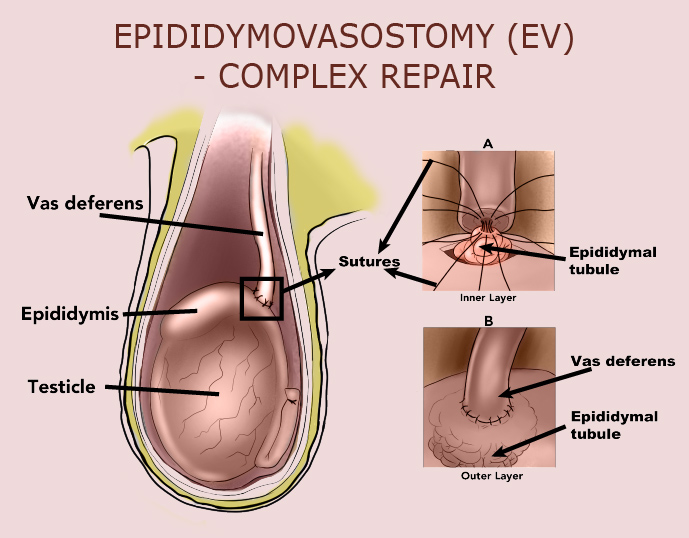
- Epididymovasostomy (EV): the vas deferens are attached directly to the epididymis (a small organ at the back of each testicle that holds sperm
What are vas deferens?
Vas deferens is the name of the tubes that sperm travel along from the testicles to the semen (see diagram below). During a vasectomy, a surgeon cuts the tubes to prevent the flow of sperm to the semen and their presence in the ejaculate. During a vasectomy reversal, the vas deferens are reconnected.
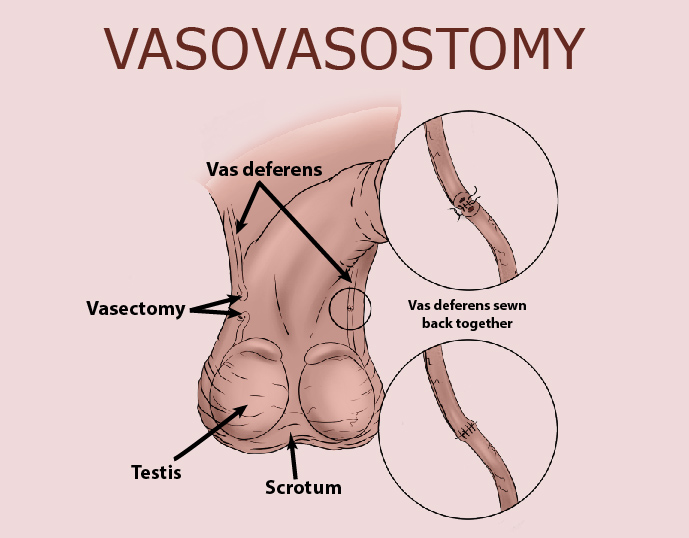
Vasectomy reversal is a more difficult surgical procedure than a vasectomy. With microsurgery, an experienced surgeon uses a powerful surgical microscope to magnify the vas deferens up to 40 times its actual size. The type of repair necessary on each side depends on whether the fluid quality from the vas deferens is optimal and whether sperm are found still making their way up the vasectomy site, among other factors. Choosing a microsurgeon that can perform both types of repair greatly improves the likelihood of success, regardless of the number of years since the vasectomy.
What does vasectomy reversal surgery entail?
Vasectomy reversal is a more difficult surgical procedure than a vasectomy. With microsurgery, an experienced surgeon uses a powerful surgical microscope to magnify the vas deferens up to 40 times its actual size.
A surgeon typically uses general anesthesia during surgery. All patients receive a local anesthetic that eliminates the pain and numbs the area.
During the surgery, the surgeon makes a small incision on the scrotum to expose the vas deferens and release them from the surrounding tissues. Next, the surgeon cuts open the vas deferens and examines the fluid inside. If sperm are present in the fluid, the ends of the vas deferens can be reconnected to reestablish a passageway for the sperm to travel.
If the fluid contains no sperm, the cause may be scar tissue or a secondary epididymal obstruction (called an epididymal blowout). Either occurrence may be blocking the flow of sperm. If this is the case, the surgeon may do an epididymovasostomy (EV).
What is an EV, and why and when does a surgeon decide to do an EV?
An epididymovasostomy (EV) is a more complicated procedure than a vasovasostomy (VV). The surgeon generally chooses this option only if a vasovasostomy cannot be done for various reasons or a VV is likely to be unsuccessful. The surgeon’s decision often depends on whether sperm are seen when fluid from the vas deferens is analyzed during the surgery. Therefore, the surgeon decides which of the two procedures (VV or EV) is needed during the surgery. Sometimes a combination of both procedures is required. For example, a vasovasostomy is sometimes needed on one side, and an epididymovasostomy is required on the other.
A surgeon’s considerations prior to recommending a vasectomy reversal
Before a vasectomy reversal surgery, the surgeon will:
- Take a medical history and perform a physical exam. This will ensure the surgeon that no health concerns could complicate surgery.
- Check to see if healthy sperm can be produced. For most males, having fathered a child before is proof. After a vasectomy, testicles continue to produce sperm, however, the amount of sperm produced may have decreased over time. Age, diet, smoking, and exercise, among other variables, can change how much healthy sperm is produced. Your surgeon may want to perform some tests before surgery.
- Confirm that the patient knows if the chosen partner can have a child. This ensures that the patient’s fertility expectations align with all parties involved.
What is the success rate of Vasectomy Reversal?
Success rates for a vasectomy reversal should not be confused with pregnancy success rates after a reversal. Patients need to keep this in mind when evaluating success figures.
Success rates for vasectomy reversal refer to the restoration of sperm in the semen. Success depends on the male’s medical history, the location and length of the vasectomy, as well as the size and firmness of the epididymis (which is assessed during the physical exam).
Success can also depend on the time since the vasectomy. All these factors should be assessed and discussed in detail with a couple at the initial consultation before choosing a surgeon.
Vasectomy reversal success rate factors by year |
||
Vasectomy reversal success rate after 5 years |
Vasectomy reversal success rate after 10 years |
Vasectomy reversal success rate after 15 years |
|
On average, at 5 years, over 95% of males will successfully return sperm to the ejaculate. |
After 10 years, the success rate is around 80%-90%. |
When the vasectomy interval is over 15 or 20 years, success rates will be lower but remain around 50%. |
Pregnancy success rates after a vasectomy reversal
Pregnancy rates after vasectomy reversal can range from about 30% to over 90% depending on many different variables: the surgeon’s experience, the type of vasectomy reversal procedures done, the partner’s fertility, and whether the male had fertility issues before the initial vasectomy.
Remember, estimated success percentages for vasectomy reversals are not pregnancy success rates. A male can have restored sperm in his semen with a vasectomy reversal, but pregnancy success always involves his female partner.
Pregnancy can only occur after a successful vasectomy reversal if the female partner is fertile and can achieve pregnancy with the sperm count that appears after the vasectomy reversal.
Good prognostic factors on the female side include:
- Prior pregnancies
- Normal menstrual cycle
- Age less than 40
- Normal AMH levels, which indicate good ovarian reserve
What is the Average Time to Get Pregnant After a Vasectomy Reversal?
Approximately 6-8 weeks after vasectomy reversal surgery, the surgeon will examine your semen under a microscope to see if sperm is present. When surgery is successful, sperm will typically be present during this exam. However, the appearance of sperm can sometimes take a year or more if a bilateral epididymovasostomy was necessary.
The time to pregnancy after a vasectomy reversal is typically at least six months. Unless a pregnancy occurs, the only way to know for sure if a male’s vasectomy reversal was successful is to check the semen. Therefore, multiple semen analyses may need to be done over time.
Even if a vasectomy reversal is successful, achieving pregnancy depends on various factors, including the number and quality of the sperm present in a male’s semen and the female partner’s age and fertility.

Choosing to extract and freeze sperm
Sperm extraction and freezing (cryopreserv ation) are important considerations in a vasectomy reversal surgical procedure. Banking sperm provides a backup plan in case the surgery is unsuccessful. Cryopreservation will allow the patient to father a child through assisted reproductive technology (ART), such as in vitro fertilization (IVF), if pregnancy is not obtained after a reversal.
Sperm can be retrieved directly from the testicle during surgery in a procedure called testicular sperm extraction (TESE). This is recommended for all men undergoing a reversal because the reversal success rate is never 100%. The average success is around 90-95% across all time frames since the vasectomy.
Vasectomy reversal risks
Vasectomy reversal rarely leads to severe complications, but as with any surgery, there are risks. These include:
- Bleeding within the scrotum. If some bleeding inside the scrotum occurs, it can lead to a collection of blood (hematoma) that causes painful swelling. The risk of hematoma is significantly reduced by following the surgeon’s instruction to use scrotal support, applying ice packs after surgery, and resting for the designated time. Your surgeon will also likely recommend avoiding aspirin or other blood-thinning medications before and after surgery.
- Infection at the surgery site. This is very uncommon, but infections are a risk with any surgery and may require treatment with antibiotics if one occurs.
- Chronic pain. Chronic pain after vasectomy reversal is uncommon. If this occurs, the surgeon will present pain treatment options.
Post-surgery care
After the surgery, patients wear tight-fitting undergarments such as an athletic supporter to support the scrotum and hold the gauze in place. The patient should not drive himself home after the procedure.
You should apply ice for 24 to 48 hours to reduce swelling. For the first 24 hours after surgery, the patient should avoid getting the surgery site wet.
You may be sore for several days and should limit activities that might cause the testicles to move around too much. As the anesthetic wears off, the patient may feel pain or discomfort. For most males, the pain does not feel severe and improves after a few days to a week. The stitches dissolve in about two weeks.
You should wear an athletic supporter for several weeks after surgery except while showering. You should also avoid any activity that might pull on the testicles or scrotum, including running, biking, heavy lifting, and other sporting activities, for at least 2-3 weeks after the surgery.
If your work entails sitting at a desk, you may resume work a few days after surgery. However, if your job involves physical labor, driving, or a lot of walking, it is essential to talk to the surgeon about when it is safe to return to work. Taking a whole week off work is the best plan for most men.
It is also important not to have sexual intercourse or ejaculate for at least a week after surgery.
What if the vasectomy reversal doesn’t work?
Vasectomy reversals are sometimes unsuccessful if there is an underlying issue with a testicle that is not detected during the surgery or if blockage develops after the surgery. Some men will have anti-sperm antibodies that immediately attack the reversal site and cause obstruction. Some men will have the surgery repeated; however, success rates are slightly lower for the second attempt.
In cases where a vasectomy surgery fails, there are options for pursuing pregnancy. Your fertility specialist will discuss all possibilities with you.
The Atlantic Reproductive Difference
At Atlantic Reproductive Medicine, fellowship-trained reproductive urologist and microsurgeon Dr. Matt Coward has over 10 years of experience performing vasovasostomy (VV) and epididymovasostomy (EV) vasectomy reversals using a state-of-the-art operating microscope. Dr. Coward performs the procedure in the comfortable setting of a reproductive medicine center in a fully outfitted male fertility operating room with the help of a dedicated anesthesia and nursing team. The total cost of a vasectomy reversal procedure at Atlantic Reproductive Medicine with Dr. Coward is $9,875, regardless of whether VV or EV is required on either or both sides. There are no hidden costs, and the price includes anesthesia as well as simultaneous sperm banking of testicular sperm (TESE).

Travel to Atlantic Reproductive Medicine is convenient, and the Raleigh area is inviting. The office is only ten minutes from Raleigh-Durham International Airport and is centered in the Research Triangle, known for its biotech companies and three top-tier universities (UNC, Duke, and NC State). World-class hotels, museums, restaurants, walking trails, and more, make visiting the Raleigh area enjoyable.
At Atlantic Reproductive Medicine, patients receive the level of fertility expertise provided at top medical institutions in a private setting offering a personal and tailored approach.
Learn all about Atlantic Reproductive Medicine by reading through our website.
If you are interested in scheduling a consultation for a vasectomy reversal with Dr. Matt Coward, click here: https://www.atlanticfertility.com/request-a-male-patient-appointment/
Male Fertility Treatments

Causes of Male Infertilty
A common misconception is that an infertility problem usually lies with the female. The reality is that half of all infertile couples have a contributing male factor.

Vasectomy Reversal
Vasectomy reversal is a surgical procedure to undo a vasectomy and when done by a skilled surgeon it is successful on most men.

MicroTESE
Microsurgical testicular sperm extraction (microTESE) retrieves sperm from the seminiferous tubules of a male’s testes in men with non-obstructive azoospermia.
No-Scalpel, No-Needle Vasectomy
No–scalpel, no-needle vasectomy is the least invasive form of vasectomy, a safe and effective form of birth control for males who are confident they do not want to father a child in the future.

Semen Analysis
Semen analysis evaluates the quality and volume of a sperm in semen. It is one of the first steps to detect male infertility issues.

Azoospermia & Abnormal Semen Quality
Azoospermia is the absence of sperm in the ejaculate. Abnormal semen quality in ejaculate refers to quality issues with sperm in the semen that can make the sperm unable to achieve fertilization of an egg.

Varicocele
A varicocele is a dilated vein within the scrotum which holds and protects the testicles. It can occur in one or both testicles and can cause male infertility.

Ejaculatory Dysfunction
Ejaculatory dysfunction is among the most common sexual disorders but there are many solutions, including medications, assistive neurostimulatory methods, and surgical sperm retrieval.

Sperm Selection
Sperm selection can separate highly motile, normal sperm from those of lower quality which is critical for fertility treatments such as intrauterine insemination (IUI), in vitro fertilization (IVF), or intracytoplasmic sperm injection (ICSI).

Sperm Retrieval
Sperm retrieval (harvesting) is done to find and retrieve sperm from the testis or epididymis in men who want to achieve pregnancy but have no sperm in their ejaculate.

 “At Atlantic Reproductive Medicine, my patients receive the level of fertility expertise provided at top medical institutions, in a comfortable, private setting. Our vasectomy reversals are done on-site within our modern reproductive medicine center, in a male fertility operating room outfitted with a state-of-the-art operating microscope. We perform whatever reversal type is necessary, including both vasovasostomy (VV) and epididymovasostomy (EV) reversals, and the competitive, all-inclusive cost includes general anesthesia and simultaneous sperm banking of testicular sperm (TESE) in our unrivaled andrology laboratory.” –
“At Atlantic Reproductive Medicine, my patients receive the level of fertility expertise provided at top medical institutions, in a comfortable, private setting. Our vasectomy reversals are done on-site within our modern reproductive medicine center, in a male fertility operating room outfitted with a state-of-the-art operating microscope. We perform whatever reversal type is necessary, including both vasovasostomy (VV) and epididymovasostomy (EV) reversals, and the competitive, all-inclusive cost includes general anesthesia and simultaneous sperm banking of testicular sperm (TESE) in our unrivaled andrology laboratory.” –