Varicoceles
What is a varicocele?
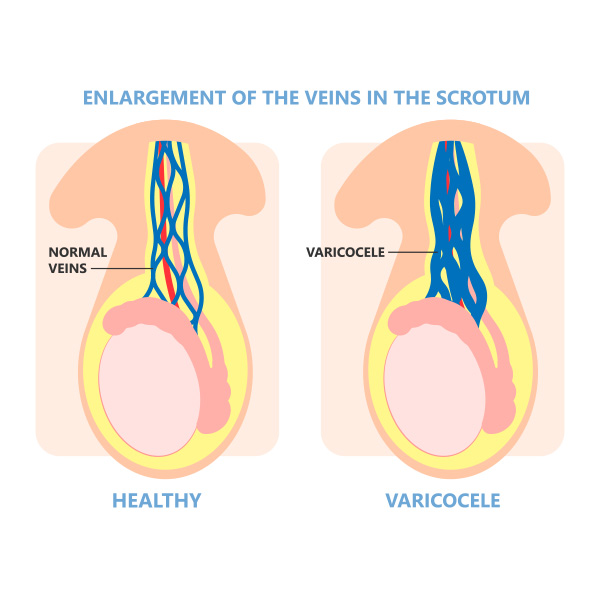
A varicocele (VAR-ih-koe-seel) is a dilated vein within the scrotum, the bag of skin that holds and protects the testicles (balls). It can occur in one or both testicles. For infertile men, bilateral varicoceles are more common than unilateral ones. The overall condition is referred to as varicocele and is often asymptomatic.
The veins within the scrotum transport oxygen-depleted blood from the testicles back to the heart, where the blood receives oxygen. The development of varicocele can result in blood pooling in the veins instead of moving efficiently out of the scrotum.
Varicocele is a common condition and a main cause of male infertility
Varicocele is a common disorder, affecting 15-20% of all males, 1 in 5. It is the most common cause of an abnormal semen analysis. Varicoceles often form during puberty and grow over time. They can cause periodic or chronic discomfort or pain, but sometimes they have no symptoms or complications. A male may not even know he has a varicocele for many years. However, varicoceles can cause poor development of a testicle, low sperm production, or other issues that can lead to infertility.
Varicocele repair can improve sperm quality for over two-thirds of men, and one-third of couples conceive naturally after varicocele treatment. With repair, assisted reproductive technology (ART), such as in vitro fertilization (IVF) and intrauterine insemination (IUI) are more likely to be effective due to improved sperm quality.
“Repair of a varicocele results in significant improvements in sperm quality for a majority of men, and one-third of couples conceive naturally after varicocele repair. Varicocele repair works best in the broader context of other fertility treatments as well, because IUI and IVF are both almost twice as likely to result in pregnancy due to the improved sperm quality after varicoceles are repaired.” – Matt Coward, MD
What are the symptoms of varicoceles?
Varicoceles usually occur on the left side of the scrotum. Less commonly, they can occur in the right scrotum. For men with infertility, bilateral varicoceles occurring in both the left and right sides is the most common. As noted above, varicoceles sometimes produce no symptoms at all, but common signs and symptoms often include:
- Differently sized testicles. The testicle that has a varicocele may be noticeably smaller than the other testicle that is not affected.
- A mass in the scrotum. If a varicocele is large enough, a wrinkled mass may be visible above the testicle. This can look like a small sac of spaghetti. Smaller varicoceles tend to be too small to see but they can be felt.
- Pain. Varicoceles can cause dull, aching pain or discomfort, more likely when standing, or later in the day as one tires. Lying down often relieves the pain.
- Infertility. Not all varicoceles cause infertility, but some do. Close to half of all men who seek medical assistance for male infertility have varicoceles.
A number of conditions can contribute to pain, a mass in the scrotum, or swelling. It is important to see your healthcare provider if you are experiencing any of the conditions or if you are experiencing infertility (having tried for a year or more to achieve pregnancy without success).
What is the cause of varicocele?
The exact cause of varicocele is unknown. One cause may be the malfunction of the valves inside the veins that keep blood moving in the right direction as occurs with varicose veins in the legs or other parts of the body.
The fact that varicoceles develop more often in the left testicle could be because the left testicular vein follows a slightly different path than the vein on the right side, making it more susceptible to the condition.
Medical researchers believe that many cases of varicocele are congenital (occurring at birth). Often varicocele is not detected until puberty when blood flow to the genitals increases and a varicocele prevents the testicle from growing properly.
What are the complications of varicoceles?
While medical experts do not fully understand the exact role that varicocele plays in male infertility, they do know that having varicocele can make it difficult for your body to regulate the temperature of your testicles and that oxidative stress and the buildup of toxins can result. These conditions may be factors that lead to the following complications:
- Infertility. Varicocele does not necessarily cause infertility but it can. An estimated 10% to 20% of men diagnosed with varicocele experience infertility. Among men with fertility problems, about 40% have varicocele.
- Poor testicular health. For boys going through puberty, varicocele may hinder hormone production and testicle growth, among other factors related to the health and function of the testicle. For men, varicocele can result in the gradual shrinkage of the testicle due to tissue loss.
How is a varicocele diagnosed?
A physical exam is typically the way varicocele is diagnosed. To confirm a diagnosis, an ultrasound test is sometimes done to provide more details of the testicular veins. A semen test or blood test is usually done to determine varicocele’s effect on fertility.
What are the treatment options for varicocele?
Microsurgical subinguinal varicocele repair
Microsurgical subinguinal varicocele repair is the gold standard surgical technique with the highest success rate, lowest complication risk, and quickest recovery time.
This surgery is done as an outpatient procedure under general anesthesia. A urologist (doctor specializing in male reproductive organs) clips or ties off the testicle veins that are causing symptoms. The surgery stops blood from flowing through those veins, eliminating the problem of blood pooling. Other veins accommodate the blood flow instead and blood is moved more efficiently out of the scrotum back to the heart.
The surgery takes about 90 minutes for each testicle treated. If both testicles are treated, known as a bilateral, the time for the procedure is about 3 hours. Most patients do not need narcotic pain medicine for the procedure.
Most males can resume exercise and sexual activity in 1-2 weeks. Varicoceles may still be felt after surgery, but the veins will no longer be connected to the rest of the body and should no longer cause pain or harm to sperm production.
Many males choose to have this surgery to improve fertility, while others may need it to reduce pain. Clinical studies indicate that sperm numbers and motility (a sperm’s ability to reach an egg) can improve after surgery and increase the ability of sperm to fertilize an egg by 40-50%.
A semen sample will be reexamined 4 months after the surgery. Around 79% of males see sperm count and sperm health improvement.
Embolization
An alternative to surgery is embolization. This is a vascular procedure done by a radiologist. Statistically, embolization has a much higher failure rate and a higher complication rate than microsurgical subinguinal varicocele repair. For these reasons, infertility surgeons generally reserve embolization for very special and very rare situations like reoccurrence of varicoceles after surgery or for those that cannot undergo surgery.
During an embolization, a vein is blocked by the radiologist. Following imaging on a monitor, the radiologist inserts a tiny tupe into a vein in the groin or neck. The tube is guided to the treatment site in the groin. The radiologist then releases coils or a solution that causes scarring. This scarring creates blockage in the testicular veins, essentially choking it off.
A local anesthetic is given at the insertion site before the procedure. A sedative may also be given to reduce discomfort and induce relaxation. The entire procedure takes about one hour. Recovery time is relatively short and with only mild pain that subsides with time. An individual can typically return to work in 1 to 2 days and resume exercise after about a week.
Varicocele repair and IUI vs. IVF
Many patients seeking fertility treatment with unilateral or bilateral varicoceles, will be faced with a decision: to repair the varicoceles or consider IUI or IVF. It is important to keep in mind that varicocele and assisted reproductive technology (ART) methods are on parallel tracks towards the same goal, but they get there at different times and with different costs and treatment burdens.
A couple can look at the decision as a difference between playing a short game (IVF) vs. a long game (varicocele repair). While IVF can result in a pregnancy relatively quickly, a unilateral or bilateral varicocele repair can take 6-12 months to achieve pregnancy. Initial signs of improvement can be seen in 3-4 months, but in the 6-9 month range more lasting results are apparent. Pregnancy rates typically go up in the 9-12 month range after the surgery.
It is important to keep in mind that varicocele and IUI or IVF treatments often work together, and sometimes both are necessary to achieve the desired fertility outcome. Often a varicocele will be fixed and then a couple still needs to proceed to IVF. It is not always an either/or decision. The physician team at Atlantic Reproductive Medicine Specialists work together to help each individual couple chart their own path. Sometimes varicocele repair is recommended initially, sometimes ART, and sometimes both. Each couple’s journey will be slightly different when varicocele is involved.
Another treatment consideration is insurance coverage. Varicocele surgery is typically covered by insurance plans, often making it more cost-effective. It also allows for natural conception in addition to improving IUI and IVF success rates by nearly double. Statistically, one-third of couples conceive naturally after varicocele repair. Two-thirds still need ART.
Finally, the age and health of the female partner must also be taken into account. Varicocele repair is much more likely to be recommended for a 30-year-old couple than a 40-year-old couple because the 40-year-old couple is more likely to need IVF or IUI anyway.
Varicocele is an important cause of elevated sperm DNA fragmentation
Another important variable of sperm health comes into play with the timing of treating varicoceles: DNA fragmentation. Sperm DNA fragmentation (SDF) refers to abnormal genetic material within the sperm. High DNA fragmentation can cause miscarriage, poor fertilization, poor embryo development, and IVF failures.
The occurrence of DNA fragmentation can be higher for men with varicoceles. If a male has varicoceles and is also found to have high DNA fragmentation, it is best to address the varicoceles before ART. Doing so improves overall testicular function most of the time. This, in turn can improve fertility success on multiple fronts.
Suppose sperm DNA damage continues despite varicocele repair, lifestyle modification, and other interventions. In that case, there are other methods, such as micromanipulation-based sperm selection or testicular sperm extraction, that can be used to select healthy sperm with improved DNA integrity for IVF.
Testosterone levels may also improve after varicocele treatment
A male’s testosterone level is yet another variable that can improve after varicocele treatment. Testosterone is made in the testicles and is needed for sperm production. If a male’s testosterone is too low, the result can be a very low sperm concentration or a complete absence of sperm in the semen.
Testosterone levels typically increase by 150 ng/dL on average after varicoceles repair. While it is not the first line of treatment for low testosterone, it can make a long-term difference.
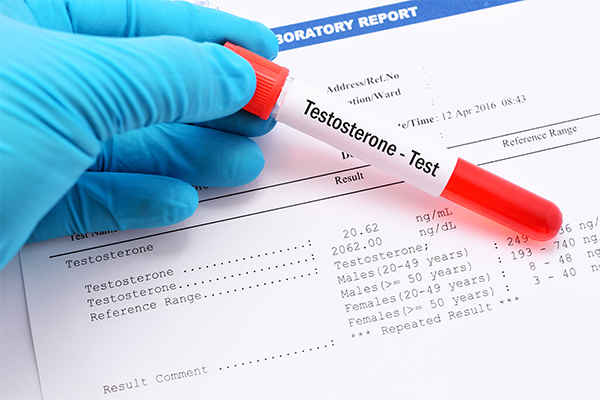
Testosterone levels vary considerably among men. Typically, older men tend to have lower testosterone levels than younger males, with testosterone levels gradually declining with age, about 1% a year after age 30 on average.
A blood test is the only way to diagnose a low testosterone level. Some males have a low level without any signs or symptoms. Many men with infertility will have a borderline or low testosterone level.
Varicocele treatment may be the end, or the beginning, of other treatments
In sum, varicocele treatment can impact several variables causing infertility. In some cases, it will resolve infertility. In other cases, more treatments may need to be done. Therefore, the path to an infertility solution will likely involve a physical exam and medical history intake, many different tests, and blood labs, all needed to piece together the best and most effective treatments.
Infertility consultations address the unique concerns of each patient
If you are concerned about infertility, set up a consultation with an Atlantic Reproductive Medicine Specialist provider to determine what next steps are right for you.
The Atlantic Difference
With the only fellowship-trained specialist in the region offering surgery for varicocele, Dr. Matt Coward at Atlantic Reproductive Medicine is able to offer our patients the most advanced procedures for varicocele surgery. If you are interested in learning more about vasectomies or any fertility or infertility issue, call us today for a consultation @ (919) 248-8777.
Male Fertility Treatments

Causes of Male Infertilty
A common misconception is that an infertility problem usually lies with the female. The reality is that half of all infertile couples have a contributing male factor.

Vasectomy Reversal
Vasectomy reversal is a surgical procedure to undo a vasectomy and when done by a skilled surgeon it is successful on most men.

MicroTESE
Microsurgical testicular sperm extraction (microTESE) retrieves sperm from the seminiferous tubules of a male’s testes in men with non-obstructive azoospermia.
No-Scalpel, No-Needle Vasectomy
No–scalpel, no-needle vasectomy is the least invasive form of vasectomy, a safe and effective form of birth control for males who are confident they do not want to father a child in the future.

Semen Analysis
Semen analysis evaluates the quality and volume of a sperm in semen. It is one of the first steps to detect male infertility issues.

Azoospermia & Abnormal Semen Quality
Azoospermia is the absence of sperm in the ejaculate. Abnormal semen quality in ejaculate refers to quality issues with sperm in the semen that can make the sperm unable to achieve fertilization of an egg.

Varicocele
A varicocele is a dilated vein within the scrotum which holds and protects the testicles. It can occur in one or both testicles and can cause male infertility.

Ejaculatory Dysfunction
Ejaculatory dysfunction is among the most common sexual disorders but there are many solutions, including medications, assistive neurostimulatory methods, and surgical sperm retrieval.

Sperm Selection
Sperm selection can separate highly motile, normal sperm from those of lower quality which is critical for fertility treatments such as intrauterine insemination (IUI), in vitro fertilization (IVF), or intracytoplasmic sperm injection (ICSI).

Sperm Retrieval
Sperm retrieval (harvesting) is done to find and retrieve sperm from the testis or epididymis in men who want to achieve pregnancy but have no sperm in their ejaculate.